Oncology-Hematology
Devoted to the study and treatment of any blood disease, particularly neoplastic or cancerous diseases, such as Lymphoma.The Oncology-Hematology Department at Instituto Oncológico Teknon is devoted to the study and treatment of any blood disease, particularly neoplastic or cancerous diseases, such as Lymphoma.
Fortunately, advancements during the last decade have permitted the branch of Hematology-Oncology to become a leading area in effective treatments, so that many of these type of diseases can be cured if a grave prognosis has not yet been determined.
- What is hematology?
In the blood we find several types of cells:
- Red blood cells, whose main purpose is the transport of oxygen to the tissues.
- White blood cells, which fight infections
- Platelets, which are important in blood clotting.
All these blood cells are produced in the bone marrow, and then enter bloodstream.
Hematology is the branch of Medicine that studies blood diseases. Thus, as hematologists, we treat the diseases of the red blood cells (decrease: anemias; increase: polycythaemia), as well as those of the white blood cells and platelets. Furthermore, there are other diseases that hematologists treat and that originate in the lymph nodes: lymphomas.
- Most common hematologic diseases
Listed below are the most common hematologic diseases, which can be properly diagnosed and treated in our Hematology Department:
- Non-Hodgkin's lymphoma
- Hodgkin's disease
- Chronic lymphocytic leukemia
- Hairy cell leukemia
- Multiple myeloma
- Waldenström's disease
- Chronic myeloid leukemia
- Polycythemia Vera
- Essential thrombocythemia
- Idiopathic myelofibrosis
- Myelodysplasia - Refractory anemias
- Bone marrow aplasia - Paroxysmal nocturnal hemoglobinuria
- Acute leukemias (lymphoblastic and myeloblastic)
- Lymphoma
- What is?
It is a cancer, i.e. an abnormal cell growth forming a tumour, which develops within the lymphatic system.
The lymphatic system contains a network of vessels, or thin tubes, connecting certain organs called lymph nodes. We can find them particularly in the armpit, groins, neck, thorax and abdomen and they can sometimes be felt when they are inflamed by an infection.
The lymphatic system carries whitish liquid called lymph, which contains lymphocytes. These are white blood cells, which have an important role in infection control since the immune system, of which it is part, is responsible for the defence of the body against external aggressions.
The lymphoma is a tumour caused by the abnormal growth of lymphocytes and it can appear in a lymph node or in another location.
- Types
There are several types of lymphomas and classification is based on differences among them: by origin, by location or by connection with other important organs . This is an essential aspect because depending on the specific type, the aggressiveness of the lymphoma and prognosis are different.
However, a simple classification could be:
Hodgkin's lymphoma: It is characterized by the appearance of lymph nodes in different parts, mainly the thorax. With an adequate treatment, the prognosis is usually good.
Non-Hodgkin's lymphoma A group of over 30 different diseases that can be grouped as follows:
It is important to note that when we mention the aggressiveness of a lymphoma, we refer to the intrinsic malignant character thereof, not necessarily to the extent of the disease. Thus, indolent lymphoma has usually spread but it still has a quite favourable prognosis. Aggressive lymphomas usually respond to the treatment and can be cured.
- Aggressive lymphomas
These represent approximately half of all the non-Hodgkin's lymphomas. Their rate of growth is very rapid. They are characterized by lymph node inflammation, but they can also infiltrate other organs as metastasis. In spite of their clinical aggressiveness, they are more sensitive to treatment than indolent lymphomas, so that most of them can be cured with the proper treatment. - Indolent lymphomas
They represent approximately 40% of non-Hodgkin's lymphomas. Their rate of growth and aggressiveness is low, but they have usually spread considerably by the time of the diagnosis. They need to be continually monitored by a doctor because in some cases, they become aggressive. Although patients with indolent lymphoma can live many years, this lymphoma can, paradoxically, be difficult to cure. - Highly aggressive lymphomas
These represent approximately 10% of all non-Hodgkin's lymphomas. The rate of tumour cell growth is very rapid, so that the number of cells (and, thus, the mass of the tumour) may double within 24 hours. They are equivalent to acute leukemia, therefore require radical and immediate treatment. In addition to the lymph node inflammations, other organs such as the bone marrow and the nervous system may also become affected.
- Aggressive lymphomas
- Causes
In most cases, the causes of lymphoma are not well known. We do know that people with immunity deficit, whether genetic,or acquired (by the AIDS virus, patients with organs transplanted, etc) are at a higher risk. Although the primary cause is not known, we are learning more and more about cellular and molecular mechanisms that lead to a lymphoma.
Within a few years, genetic risk factors are likely to be determined, i.e. if one newborn would be more predisposed to develop a lymphoma than another.When genetic factors are known, we will be able to act before the lymphoma appears and prevent it.
- Who does it affect?
Any person can have a lymphoma. Although, in general, they affect men and elderly people, lymphomas can appear at any stage of life.
- Symptoms
The most common is lymph node swelling, which is known as "adenopathy". You may not necessarily feel other symptoms and that is why it may not be noticed easily.
Sometimes, aggressive and very aggressive lymphomas do cause symptoms, such as weight loss, lack of appetite, temperature, profuse sweats or fatigue.
Lymphadenopaties usually appear in the neck, the armpits or the groins. Sometimes, the size of the liver and the spleen may be enlarged. Other times, the lymphoma affects organs such as the stomach, bones, lungs, brain or testicle.
Whenever a swollen lymph node appears, i.e. a person feels "a lump", wherever it is located, it is important to see the doctor so that he/she can assess and determine if a test is needed, though the most common cause for an adenopathy is an infection, trivial in most cases.
- Diagnosis
Lymph node biopsy
This technique is used to diagnose a lymphoma.
It involves the microscopic study of the tissue of the involved node. Perfoming a biopsy, a sample or perhaps even the whole adenopathy will be removed. In general, a small surgery with local anesthesia will be needed. It does not produce considerable discomfort, especially if the node is external. A biopsy of the internal nodes or other organs such as the stomach or liver is seldom needed.
Biopsy is the only way to diagnose lymphoma and to determine the type.. Therefore, it is essential to decide which treatment is to be followed.
Extension study
Once the diagnosis is performed, additional examinations must be done to determine the extent of the disease. THis is called extension study of the lymphoma and it consists of the following tests:
* complete blood test
* thoracic X-rays
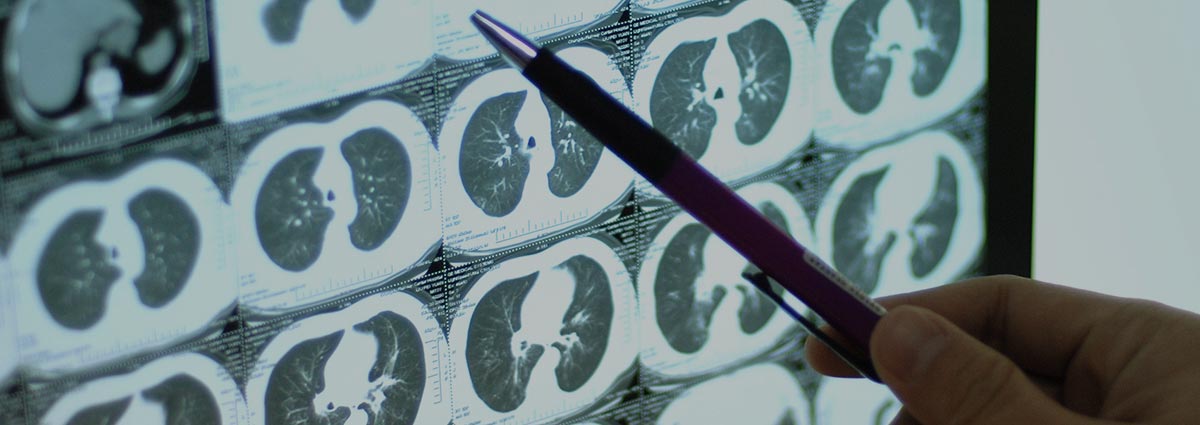
* Computed Tomography, also called CT scan of thorax, abdomen and pelvis
* bone marrow biopsy
and in some cases:
* nuclear magnetic resonance
* nuclear scan
* fibrogastroscopy, fibrocolonoscopy or fibrobronchoscopyBy means of the biopsy and the additional tests, the doctor can assess the condition of the organs and the stage of the disease, so that he/she can establish a treatment
In order to quantify the extent of the disease, we use the Ann Arbor classification, which defines four degrees in the condition or stages (from I to IV):
I. a single node region
II. two or more node regions confined to one side of the diaphragm
III. two or more node regions spread to both sides of the diaphragm
IV. involvement of other extra lymphatic organs (what in other types of cancer is called metastasis) - Treatment
Once the type of lymphoma and the degree of extension (stage) is determined, the treatment can be started. The specialist will assess each particular case to determine the most appropriate treatment. There are no golden rules because each patient and his/her lymphoma is different
- Therapeutic abstention
In many indolent lymphomas, it is not necessary to act immediately. In the event that the disease is asymptomatic and the growth is very slow, the best option may be to not have any treatment until more symptoms appear . This is called therapeutic abstention. Obviously, the patient must have regular medical monitoring (every 3 months, for instance) in order to determine when an active treatment is needed. Although the lymphoma may not be cured, the patient can live many years thanks to the proper monitoring. In these cases, the indolent lymphoma must be understood as a chronic disease. - Chemotherapy
This is the most common treatment because of its high effectiveness. It uses combinations of drugs that are very toxic to tumour cells and kill them, so that the lymphoma can be completely erradicated.. Although chemotherapy is used for treating most lymphomas, occassionally other treatments need to be used in conjunction with this. - Radiotherapy
This may be used to treat lymphomas in combination with chemotherapy and is given after it. There are few cases where radiotherapy is the main treatment.
It consists of giving high-dose radiation that destroys cancer cells.
The administration is local, on certain nodular regions. As in chemotherapy, there is no need for admission at the hospital. Sessions are short, lasting up to half an hour. - Biological therapies
New techniques, arising from research on how the human body works, are called biological therapies because they use substances made by the body's own cells or similar to them but made in a laboratory. The most frequently used therapies of the category used in the treatment of lymphomas are monoclonal antibodies.
Antibodies are substances produced by the immune system as an effective defense against external agents (or antigens) . They are called monoclonal because they refer to a sole B lymphocyte clone, which are the cells that produce these antibodies.. A clone means that they are cells derived from the culture of a single cell. This discovery represents a great advance because antibodies interact only with a specific antigen "target" located in the tumour cell. Thus, the lymphoma cells can be destroyed in a selective way and with low toxicity to normal cells. Rituximab (anti-CD20) is the most common monoclonal antibody. It is administered intravenously in a medical centre and there is no need for admission to the hospital. - Haematopoietic stem-cell transplant
In many highly-aggressive lymphomas and in some aggressive or indolent lymphomas, the treatment selected may be a powerful chemotherapy treatment and followed by haematopoietic stem-cell transplant, which means stem cells from the bone marrow. These cells can also be found in blood, from where they can be easily withdrawn. A transplant is performed when the chemotherapy treatment in the patient has shown good results.
The transplant is used after giving a high-chemotherapy dose to achieve the complete remission of the tumour. Such dose would damage the healthy cells in the bone marrow in a nearly irreversible way. In order to counteract this and achieve a speedy recovery, healthy cells are obtained from the body before having aggressive chemotherapy. Then, when the therapy is over, they are reinserted into the patient. Stem cells or haematopoietic cell are obtained by means of blood withdrawal and blood centrifugation. That material is frozen for later intravenous insertion (as a serum), after chemotherapy has been given . This procedure is called Self-transplant of haematopoietic stem-cells. The patient has to be admitted to hospital for approximately a month for this procedure to be performed.
In special circumstances, a haematopoietic stem-cell transplant can be done from a compatible brother or sister. This procedure is called Allogenic haematopoietic stem-cell transplant.
- Therapeutic abstention
- Living with lymphoma
Living with lymphoma involves combining your normal life with stages at which you receive a treatment.
Chemotherapy and radiotherapy may produce some discomforting side effects. They do not always appear, that depends on how your body reacts or on the duration or intensity of the treatment. There is no relation between the appearance of side effects and the effectiveness of the treatment.
These effects are just a phase and they disappear soon after the treatment. They may even not appear during the first sessions or be significant by the end of the treatment.
In some cases, your doctor may decide to stop the treatment for a few days so you can recover and continue it a few days later.
- Chronic Lymphocytic Leukemia
- What is?
Chronic lymphocytic leukemia (CLL) is the most common form of leukemia in western countries, where it is estimated that each year between 3 and 5 out of every 100,000 people learn that they have this disease. In general, CLL diagnosis is made in people with no symptoms, who are having blood tests done for other reasons (for instance, glucose or cholesterol tests) when an increase of lymphocytes (a certain type of blood cell) is detected.
The increase of lymphocytes in the blood does not indicate the diagnosis of this type of leukemia, since there are other diseases provoking cell increase, but not the special subtype leading to CLL.
- Causes
The causes of CLL are unknown. It is not considered to be a hereditary disease, since the number of family cases is around 5%. No relationship to external factors (toxic substances, radiation) has been determined.
Patients with CLL have chromosome abnormalities in diseased cells. Although we do not know which genes are involved, some of these abnormalities are essential for the prognosis and the predictable response to treatment.
- Symptoms
As previously observed, more than 80% of the cases are diagnosed by chance. The other patients who see their hematologist usually have the following symptoms: fatigue and, sometimes, temperature or weight loss and enlarged lymph nodes. Blood tests show an elevated white blood cell count and sometimes anaemia (lack of red blood cells) or thrombocytopenia (low platelet count). Other CLL symptoms, such as being more sensitive to mosquito bites, are very rare.
- Diagnosis
The diagnosis of chronic lymphocytic leukemia requires a well-equipped lab that can analyse not only the shape and size of cells, but also the antigens (proteins) that these cells have on their surface. A careful lab analysis allows to distinguish CLL from other diseases with a different prognosis and treatment. Blood enlargement in a patient with chronic lymphocytic leukemia, where a lymphocyte increase is observed (cells dyed blue)
Image analysis by flow citometry. This lab method enables the differentiation and analysis of the different types of blood cells, both in healthy people and in leukemia patients
The tests performed on all CLL patients include a general and complete analysis, the study of the membrane antigens and the study of the bone marrow (where the disease originates). In addition, in specialized centres such as ours, various studies determine the rate of aggressiveness of the disease and the prognosis. These studies include the analysis of protein ZAP-70, CD38, study of chromosome abnormalities, thoracic and abdominal CT scan, etc. After the collection of previous data, the diagnosis is performed and the prognosis is established, as well as the treatment needed.
- Prognosis
The prognosis for patients with chronic lymphocytic leukemia is variable. Whereas in some patients this type of leukemia is just an analysis discovery with no impact on the general condition of a person or on life expectancy, in other cases the CLL produces some symptoms (such as an enlargement of lymph nodes) and patients need treatment.
Therefore, it is essential to determine which patients with CLL have a more aggressive disease and which ones have a benign-type disease (so they would likely need no treatment). Our teamwork has recently identified a "marker" that is very important for the prognosis of this type of leukemia.
Global survival for CLL patients.
Global survival probability curve for CLL patients
Survival according to ZAP-70 value
Survival probability curve for CLL patients according to ZAP-70 value. Patients with low ZAP-70 values have a better prognosis than those with a high ZAP-70 value
This marker is called ZAP-70 and permits a prognosis to be made with significant accuracy.. this simple blood sample analysis technique,can determine which CLL patients would need more monitoring in order to detect any complication that may require treatment. It would alsodetermine which patientscould have a benign development of the disease and, thus, who could avoid treatment at least for a few years.
- Treatment
The CLL treatment depends on the age and the level of activity of the disease. Whereas some patients will only need periodic monitoring with blood tests, other ones will need treatment to control the disease.
There is no standard treatment for CLL patients. The ongoing trend is to administer new combinations of treatments capable of making the disease disappear in a significant number of cases. The Hematology Oncology Department in IOT is composed of nationwide and worlwide reference specialists in the treatment of this disease. Thus, new treatment methods using different chemotherapy treatments (fluradabine and the combinations thereof) are used. These advances in the treatment of CLL are very effective and do not have the disadvantages of traditional chemotherapy treatments.
Other treatment options are new biological therapies such as the use of different monoclonal antibodies such as MabCampath® (alemtuzumab) or Mabthera® (rituximab). By means of these drug combinations, a high clinical effectiveness together with a low toxicity have been achieved, allowing the patient to maintain a high quality of life.





















